
The Big C - 2022
Dealing with cancer can be a lonely place.

Cancer can be a lonely time but with care, understanding and some planning, it really does not have to be.

It’s all over now …. Isn’t it?
I’ve reached that point when people assume that my cancer
journey is over. I’ve had my first-year checks. I’m back at work, life is busy
and I am out socialising. To all intents and purposes, I look the same as I
used to and so therefore the logical assumption is, it is all over now. Move
on!
Will I lose my hair?
Coping with potential hair loss.

When I first learned I had cancer and was likely to have
chemotherapy I was understandably terrified. But what made it even worse was
the response from other people. Almost inevitably the first comment would be, ‘Oh
no, you will lose your lovely hair,’ or something similar. So, by the time I went
for my first oncology appointment I was in quite a state.

Look good feel better
Facing cancer with confidence
www.lookgoodfeelbetter.co.uk
There are so many things that hit you when you have cancer.
Dealing with the diagnosis is the first priority but then there are also the
emotional and physical changes that take place and often take you by surprise.
The chemotherapy regime is different for every case and the results are too.
Some people may experience weight loss or weight gain, some lose their hair or
it thins, others lose their confidence and motivation. Many experience feelings
of loneliness and isolation as no one truly understands how you are feeling,
your worries and fears unless they have been through something similar
themselves. It can be a difficult and uncertain time to negotiate.

Tips
Do I need counselling?
Taking up the offer of counselling and what it could do for you.
Have you ever chatted to a counsellor? Or seen the need
to? I haven’t and never really thought
it would be of use to me. I am used to talking things through with friends and
family or battling on through by myself, working things out in my own time. But
very early in my oncology journey, I was asked, ‘Would you like me to sign you
up for some counselling sessions?’ To be
honest, at that point I was in such a daze, I said yes to anything that was
offered without really thinking about it, figuring that if I changed my mind I
could stop the process at any point.
Scanxiety
So, are you back to normal now then?

Let's ring that bell!
It is amazing how quickly you get into a chemo routine. You
know roughly how you are going to feel after each session and you adjust
mentally and physically. I learned to be
very careful to avoid anything cold for the first few days, to eat what I
wanted to avoid queasiness and to rest as and when I needed to without feeling
guilty. An afternoon nap seemed to happen quite naturally and I realised this
was a good thing and gave me extra energy for the evenings.



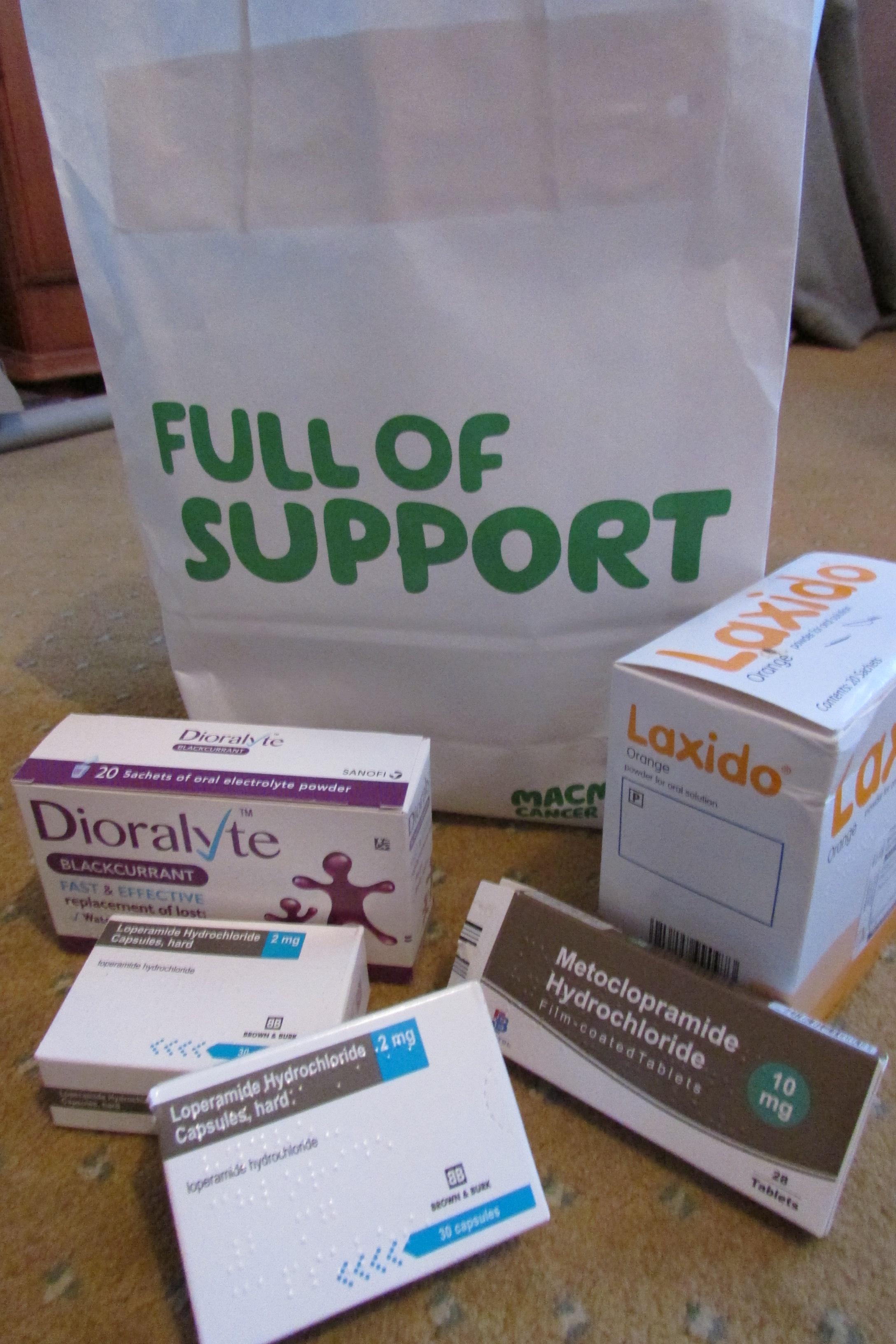
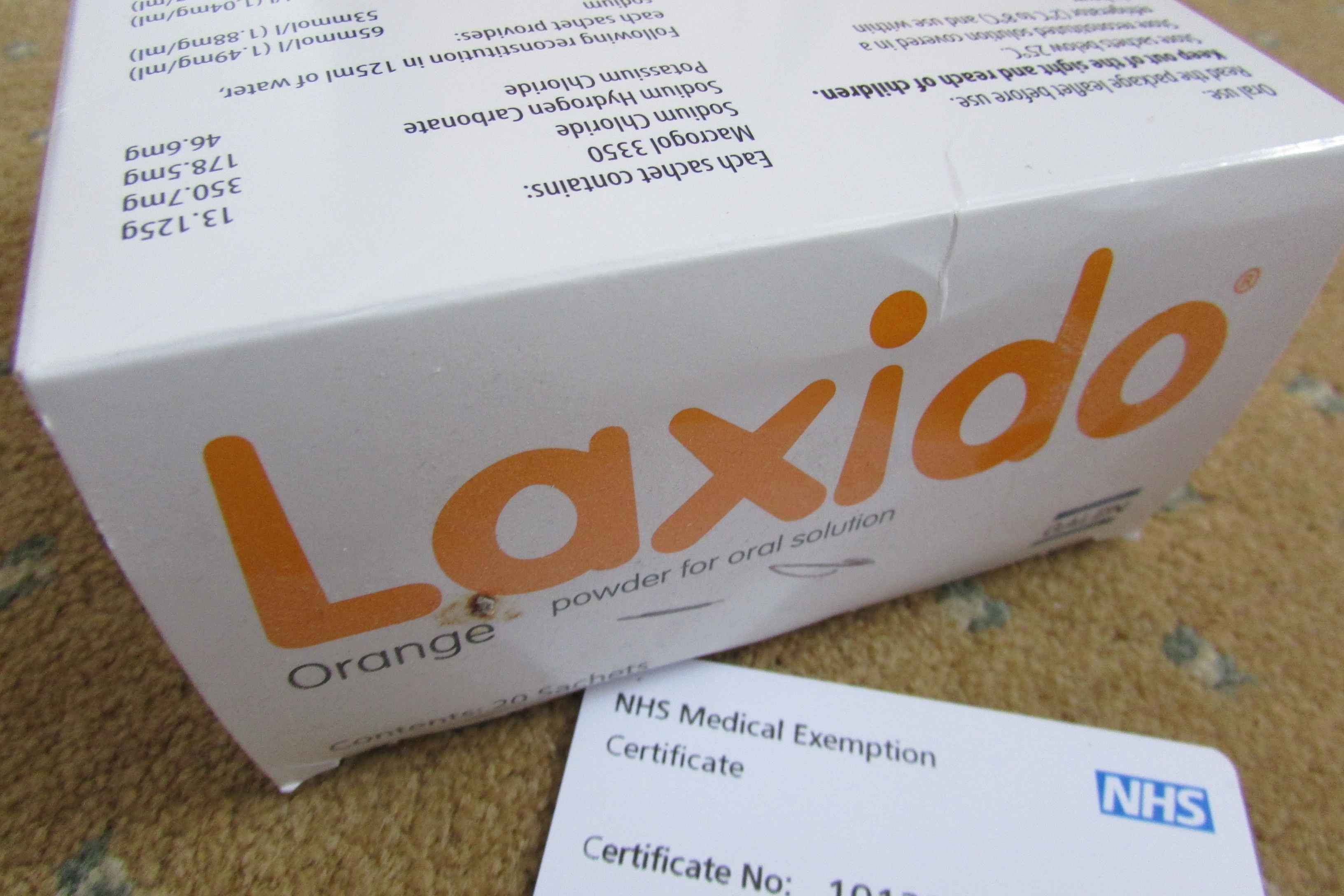
Coping with chemo after effects

Everyone going through chemo deserves a medal! It is not easy but sometimes it is not as bad
as you think it is going to be. The worst fear is in your mind and until you
are hit with it, you can never really be sure how you will react. This is my account of chemotherapy and how it
affected me. Your story is likely to be different. Even those I have spoken to
with bowel cancer like myself have had different treatments or reacted in
different ways, though there are some areas of common ground. Hopefully there
will be some useful hints for you if you are heading down the chemo route
yourself but go in with an open mind, try not to be too frightened (it is
normal to be a bit scared!) and take it one step at a time.

Chemo session number 1!
Despite a pre visit, watching a video, talking to friends and researching chemotherapy, nothing really prepared me for my first visit to the Magnolia Centre chemotherapy suite at York Hospital. There was nothing to say how my body would cope with what was going to happen or how my mind would react – it was all uncertain. There was no reason why I wouldn’t cope but until it happened, I wouldn’t know.

Preparing for chemo
Before chemo can begin, there is paperwork to sign! Lots of it! Paperwork to say that you agree to the proposed treatment, whatever it does, and are happy
to go ahead. Happy was a strange word to use I thought, I wasn't happy, I was terrified! I still had the option of not going ahead as
nobody could say whether chemotherapy was indeed necessary in my case, but the medical view
was that this was the best option to clear up any loose cancer cells that might
be floating around inside my body – a mop up of anything left behind that they
couldn’t spot with the visible eye. I honestly don’t think at this stage that
there is a real choice – perhaps if you have tried it previously and it hasn’t worked, but at
the beginning you just want to do everything you can, throw everything at the
cancer and look towards the future.
Know that you are starting on a path that will ultimately
give you the best chance of ridding yourself of cancer. It might seem a tough
journey and a huge mountain to climb, but you are taking the first steps so be
proud of yourself.
O is for oncology
Oncology. It is a word that terrified me when I was first
told that I was to report to the oncology department to discuss the next stage
of my treatment. It is a word I never thought I would be using in relation to
myself. My appointment was brought forward which would have freaked me out had
the receptionist not been very clear that a cancellation had occurred and they
were offering it to me if I wanted it and not for any other reason. She
repeated this several times so I suspect she knows that people go into panic mode!
Although it was during the pandemic, I was told I could have somebody with me
on this occasion which was a huge relief. I wasn’t sure whether to take the
appointment or not, but hubby felt that it would be good as we would find out
what we were dealing with and the way forward much quicker and perhaps
treatment would start quicker too.
Recovery time - moving on from surgery.
Recovering from major surgery (bowel reconstruction) takes
time and patience is needed! We all recover differently from surgery – some
seem to bounce back; others need longer but no one should feel pressured - it
is very much a case of being sensible, doing what you feel you can do and
perhaps setting yourself small goals when you feel up to it.

My Tips (This is what helped me, remember you may be different. Do what is right for you!)
·
So what happens after surgery?
The first few days and the first steps towards recovery.
It’s always a relief to wake up after surgery and know that
you are going to be ok! Abdominal surgery is never easy and any movement is
painful. Movement is restricted anyway as you are hooked up to various drips
and have a catheter for several days but be warned, they do get you up and
sitting in a chair as soon as possible!
In my case, it made me feel very sick pretty quickly but there is
medication to help prevent that. Ask for it if necessary. Getting up out of the
bed was also a major feat, despite support on both sides and a mattress that moves to help - it is still hard work on a very sore tummy area.
Surgery Day
What may happen on the day of your surgery.
Surgery day.
It seemed to come round rather too quickly and since I wasn’t given much
notice, I didn’t feel very prepared. However, maybe having so little notice
helped me keep calmer than I would normally have been!! Had I known for a long
time in advance, my blood pressure and nerves would have been through the roof!
POT – Pre op time!
Preparing for surgery.
I was quite glad that I didn’t get much notice of my
impending surgery because I knew that I would get into a dreadful state of
anxiety and work myself into a complete state of panic. With little notice, I
managed to remain quite calm as there was a lot to do in the few short days I
had. Whether this was due to the urgency of my condition, the availability of
the consultant/theatre time or the pandemic, I am not quite sure. The pre op
was a new experience for me and very different to the experiences of friends going through different types of cancer treatment. As such, this is an
account of my experiences (what I can remember) of a pre op in Covid
times, in preparation for the removal of a bowel tumour. If you find
yourself in similar circumstances, this might help give you an idea of what might happen.
Tips:
·
Do not be afraid to ask the medical staff to
repeat instructions so that you understand them fully.
·
Try not to worry about the testing procedure,
they are making a judgement from those, from your health background and from
chatting to you. If you forget a word for example, they are not automatically
going to announce you have dementia!!
·
Get everything written down for you so that you
can look at it again when you are feeling calm. There is nothing worse than
getting home and suddenly not being able to remember what to take and when to
take it.
·
Trust that the medical staff are doing
everything they can to ensure that you are in the best place for surgery
·
Try not to worry – easier said than done!

A testing
time ..
I am a
natural worrier. I am scared of medical procedures, mainly because I don’t know
what to expect. I have also been told many horror stories! These are not
helpful so please do bear that in mind if you know of somebody going through a
similar procedure to one you have had yourself. Below I will outline some of
the procedures I experienced, what they entail and how I felt about it, in the
hope of alleviating fears you may be having.
All cancers
are different. All are treated differently and all involve different investigations.
These are experiences I undertook towards a diagnosis of bowel cancer. Your
investigations may be completely different but hopefully you will realise that
whatever tests you have to go through, they are NEVER as bad as they are in
your mind!
What do I
say? When do I say it?
Telling people you have cancer is not an easy task. It is hard enough to accept the diagnosis when you are given it, but to then verbalise it is just weird. In my case, it felt then and still does, that I am talking about someone else, not myself. It just feels so strange to say, Hi, Just thought I’d ring and tell you I have cancer!!
I